1. Medical fees: digital capitation or fee-for-service
In the health insurance sector, the arrangement of a contracted medical network with free choice remains predominant, both in terms of premium volume and the number of insured individuals. However, the current model, based on paying professionals via a fee-for-service scale, shows clear signs of exhaustion. The relationship between insurance companies and healthcare professionals is becoming increasingly strained. The existing model incentivizes dynamics that generate dissatisfaction for both parties and, in the medium term, jeopardize the sustainability of the system.
This situation highlights the need to evolve toward a model based on new mutual collaboration, which provides greater value across three fundamental pillars:
- Healthcare improvement: enhancing the quality of patient care by, for example, providing professionals with more comprehensive and integrated clinical information.
- Professional sustainability: improving the economic conditions and the benefit framework for physicians.
- Financial efficiency: optimizing premium management by companies, ensuring the viability of the model.
It is worth remembering that capitation or per capita payment models, which were at the origin of health insurance, preceded the current system of free choice and fee-for-service, until they practically disappeared. In that model, the insured person paid a premium in exchange for receiving care within a limited and assigned network, without the possibility of choice. In return, the physician or provider received a fixed per capita amount per insured individual, typically monthly, regardless of the actual use of the service.
This system presented clear advantages and disadvantages.
- The main advantage was better control over income and expense variability for both the company and the professional.
- The main disadvantage lay in the limitation of the patient’s freedom of choice, as they were restricted to the small assigned network.
Unlike the capitation model, the current system of free choice and fee-for-service incentivizes high utilization and the reduction of unit service costs. Furthermore, since costs depend directly on the insured’s actual usage, they become variable and unpredictable. This makes it difficult to determine the loss cost in advance and, consequently, to clearly understand the income and expenditure margins for both companies and professionals.
Digital transformation now introduces new tools and capabilities that allow for a rethinking of this scenario. Thanks to better information management, clinical follow-up, and data analysis, it is possible to envision hybrid models that reclaim the advantages of the capitation system while overcoming its original limitations. This opens up an opportunity to reflect on the reactivation of an evolved capitation model, supported by digital management, aimed at two priority objectives:
- From the patient’s perspective, to respect and maintain the free choice of providers.
- From the perspective of doctors and insurers, to control costs and service compensation, reducing claims variability and improving economic predictability.
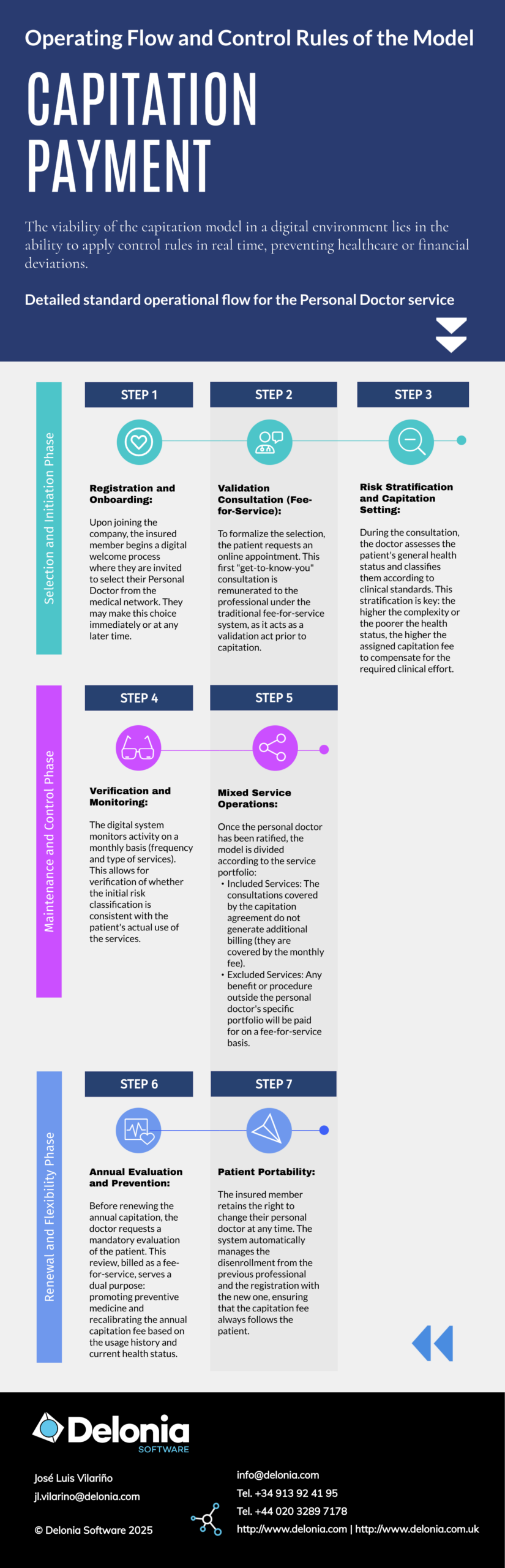
2. Characteristics of the digital capitation model
The digital capitation proposal outlines an operational framework that redefines the relationship between the healthcare professional and the insurance entity. This model is structured under the following premises:
-
Segmentation by specialty and portfolio
For high-frequency specialties, a fixed monthly payment (capitation) per insured person is established. This amount covers a specific and closed portfolio of services. Other services outside this catalog will continue to be remunerated through the traditional fee-for-service scale system.
-
Selection and assignment of the professional
The new policyholder selects (or is assigned) a reference professional or clinical unit (e.g., family doctor, pediatrician, podiatrist) within the medical network included in their policy.
-
Management of registrations and immediate communication
At the moment of assignment, the professional receives an automatic notification informing them of the new patient linked to their quota, at which point the corresponding capitation begins to accrue.
-
Flexibility and patient mobility
Through their private area, the patient has the freedom to change doctors at any time. This movement automatically generates the enrollment with the new professional and the cancellation with the previous one, updating the payment records.
-
Intelligent assignment based on patient activity
Automatic assignment systems can be implemented where, if the patient does not make an express choice, the system links them to a professional based on their activity history and actual use of the service. The assignment “follows” the patient’s activity.
-
Protocols for sporadic use
The model includes specific rules for the occasional use of other resources within the medical network (emergencies, travel during vacations, etc.). These cases are managed without implying a change in the reference professional or altering the capitation assignment.
-
Consolidation of “Favorites”
The user experience and their recurrence will progressively shape their list of regular practitioners. Those marked as favorites or frequent will be the ones who receive the capitation payment.
-
Predictability and change in professional focus
For the practitioner, this model guarantees stable monthly income, facilitating the planning of their activity. Since it does not depend on the generation of clinical activity, the professional can focus on retention and recruitment, prioritizing personalized care that does not strictly require being in-person.
-
Monitoring and renewal
The system requires annual capitation renewal mechanisms. In exchange, it establishes a mandatory requirement for the professional to conduct and record an annual clinical evaluation for each assigned patient, thereby ensuring proactive preventive monitoring.

3. Technological infrastructure of the digital capitation model
The viability of this model depends on an advanced technological platform that seamlessly integrates the private areas of patients and providers. The primary objective is for technology to act as a facilitating layer, abstracting the complexity of operational rules so that the end user perceives a simple experience focused on the following pillars:
3.1. Clinical registration and traceability
The platform must automate the recording of all healthcare activity by uploading the outpatient MBDS (Minimum Basic Data Set). This ensures that clinical information serves as the engine that validates capitation and continuity of care.
3.2. Digital management ecosystem for the professional
It is essential to provide the practitioner with an integrated toolkit that enables proactive, rather than just reactive, health management:
- Schedule management: real-time synchronized online booking systems.
- Remote care channels: Video consultation modules and telemedicine tools.
- Digital prescription: Management of electronic prescriptions and digital medical orders (lab tests, diagnostic imaging, and specialist referrals) with complete traceability.
- Omnichannel: Mobility tools and 100% online direct communication between doctor and patient.
3.3. Configuration of the mixed product
This technological foundation allows for the consolidation of a hybrid health product. Within it, the capitation system (for primary specialists) and the fee-for-service system (for specific acts) coexist harmoniously, guaranteeing the patient free access to all the resources and facilities within the company’s medical network.
Perhaps the fee-for-service model has reached its limit, which facilitates a transition toward digital capitation. This hybrid system not only stabilizes the economic relationship between insurers and professionals but also represents a vital shift in focus by promoting preventive medicine. By releasing the practitioner from the pressure of clinical volume, the model incentivizes proactive and personalized patient follow-up that builds loyalty. In a sense, digital capitation can be the key tool to ensure the sustainability of the sector, aligning financial efficiency with the ultimate clinical and economic value: long-term health.
In a future article, we will analyze in detail the specific advantages that this digital capitation model brings to each of the three stakeholders: the insurer, the patient, and the professional.